"Family members and friends of people with BPD are often desperate when they contact us", according to Barb Mullen, the Founding Director of BPD Community.
While the circumstances for every family member or friend is different, they share a common sense of uncertainty as to what they can do to make things better. Fortunately, the same solution works for everyone: BPD informed support and psychoeducation in skills and techniques to build more positive relationships. Sometimes a person attends one or two sessions and they think they have 'got it', only to return again later, as desperate as ever. It takes time and the skills learnt require practice, but the results are powerful. "There are no brave firefighters saving lives in the world of BPD, just normal people doing their best to be compassionate", said Barb.
The focus of the Family & Friends Group is to build more positive relationships with loved ones with BPD. The researchers of the Family & Friends Group conducted in depth interviews of five participants in the group, including: males and females; parents, a sibling, and a spouse. The following is a short summary of what they identified as the critical ingredients of the relational approach.
All of the quotes and observations below come from the research report compiled by researchers Anneliese Spiteri-Staines and Jasmin Isobe - Spiteri-Staines, A., & Isobe, J. (2022). Exploring relational support for the BPD community: Final project report. Melbourne: University of Melbourne.
Self-acceptance:
‘BPD Community has been a lifesaver for me. I started my journey of learning to help my [loved one] and quickly found out that change starts from within.’
Participants described the F&F group as a place where they learnt theory behind self-acceptance, strategies to tap into peace of mind and recognition of what they could control and what they could not. Although some participants spoke about this as a foundation applicable to any relational interaction, they emphasised that the particular dynamics of BPD made this absolutely essential to being able to move towards recovery, ongoing wellbeing and positive relationships with their loved one, but importantly, with themselves.
Self-acceptance and inner peace were described as essential to being able to engage with authenticity and presence with their loved ones who were particularly sensitive to inter- and intrapersonal tension or unease. The skills, strategies, and space to practice these things in the F&F group was lifechanging for participants. Radical acceptance and mindfulness practices are skills that can contribute to the development of compassion, but they are not enough on their own.
Validation and empowerment:
‘The whole approach is so empowering. It wasn’t that there was anything wrong with me or my [loved one], but there were things we could both do. […] It was so empowering for me, because I got back this power of wow, there’s all this stuff I can do, it’s not all on my [loved one] to change, that’s so out of my control. What can I do, what can I change in myself, what do I have control over and what can I work on myself right now. I went from this place of utter despair, of feeling nothing was ever going to improve, to having something to work on, trying stuff out every month, and honestly seeing huge improvement.’
Being able to focus on their own behaviour, developing their own skills and responsiveness was a profoundly impactful and ongoing experience for participants. Engaging in the F&F group allowed participants to shift their understanding of the things and actions that were under their control and that they could change, and the aspects of their relationships or circumstances that required validation and radical acceptance but that were situated outside of their control. It is the teaching of skills and techniques that can be immediately implemented that makes a difference.
community and ongoing practice:
‘When you’re kind of by yourself and going through something like that, someone who doesn’t get it, doesn’t have it, a loved one with BPD, telling you oh maybe you should change – no way, I wouldn’t have been able to hear that! No way! But when you’re in this beautiful support group, where people are hearing you, validating you, understanding how hard it is, but ALSO saying, maybe you could have communicated differently… I think that’s really specific to relationship and the kind of learning. People can hear and take on some hard truths around their own behaviour that I don’t think happens very often in other situations or types of support.’
This ongoing access and sharing of experience also helped participants with their felt sense of isolation as they navigated the changing and continuing challenges and successes of their relationships with loved ones, and themselves. Participants described having a sense of community from the group that felt unconditional, non-judgemental, and stable in a way that other friendships or support networks did not. This was a unique dynamic, where they felt validated, but also challenged in positive ways that were not part of how they were able to interact with other support networks. This allowed participants to feel open to learning, practicing and reflecting on behaviour and strategies to manage it (their own and their loved ones’), in a way that they had not had access to before.
in conclusion:
Being able to focus on their own behaviour, developing their own skills and responsiveness was a profoundly impactful and ongoing experience for the research participants. Engaging in the F&F group allowed participants to shift their understanding of the things and actions that were under their control and that they could change, and the aspects of their relationships or circumstances that required validation and radical acceptance but that were situated outside of their control. Participants spoke about feeling empowered in themselves and their actions even when a loved one may not be ready to take on changes in their behaviour, or when other family members, professionals or surrounding people were unwilling to engage with a diagnosis and presentations of BPD. The development of being able to validate and accept what could not be changed, while applying the skills and strategies they learnt to the things that could be improved, was described as a constant process of learning and practice by participants, and something they were wholeheartedly committed to. That BPD Community provided ongoing support in this is central to empowering participants and in turn positively affects recovery possibilities for the loved one with BPD.
Family members and friends of people with BPD can support recovery for their loved ones through the development of a more supportive relationship with them. They achieve this by learning to put on their own oxygen masks: to focus on giving with compassion and showing gratitude for their loved ones.
Our relationships are the cause of our greatest joy and our greatest pain. People who love someone with Borderline Personality Disorder (BPD) are often challenged in those relationships, while people with BPD experience 'relational dysregulation' as a domain of the disorder that dominates their lives. For both parties in the relationship these challenges can block recovery.
The family of a person with BPD, whether it is the natural family of birth or adoption, or whether it is a family of choice created by the person with BPD, is the primary support for a person with BPD. To support a person with BPD, it is essential to support their family so that they stop enabling the continuance of the disorder and instead support the person with BPD. When a person feels supported, recovery is an easier path.
Dr Annelise Spiteri of University of Melbourne and her assistant Jasmin Isobel, recently conducted research into the BPD Community Family & Friends Group. The extensive research project is in part, an in depth exploration of the BPD Community Family & Friends Group. The interviews with participants from the Family & Friends Group identified three themes of relational support to illustrate the experiences of the family members and friends of someone with BPD. The themes are only one aspect of the study and are described below:
Support or lack of support through mental health and medical systems
Participants described how they were overwhelmed with the enormity of the situation they found themselves within their relationships with someone with BPD and underwhelmed with how they were received within the mental health system. They were concerned with how the system treated their loved ones as well as themselves. Emphasised was the lack of knowledge, understanding and expertise in BPD as well as the unique challenges that faced loved ones of someone with BPD.
‘You might go along to a psychologist and get some medication, but that’s only treating one thing, it’s not teaching them how to cope with life and how to cope with relationships. That’s one of the bigger things. […] it’s the relationships, and the relationships are the things that cause them the most pain.’
Participants referred to the sense of isolation they felt as they tried to support their loved ones and the dismissive, often stigmatising behaviour of healthcare staff, including refusal of treatment for their loved ones when the BPD diagnosis was mentioned. An effect of this was the impact on any sense of optimism that recovery might be possible. When they did receive advice it was descried as superficial or non specific to BPD. This was compared to the in-depth learning and support received from the BPD Community Family & Friends Group.
The complete lack of support offered to family members especially to manage crises and highly complex situations was compounded when they were made to feel responsible and at fault for inadequate care and support. Families felt blamed and that they were responsible and had to 'fix' the situation.
‘I had so much interaction with emergency services, like I had so much interaction with going to hospital, and calling ambulances, and having police at my house, and this was me as a young person at the time, by myself going through all of this, and I was not offered support once by anyone. I just thought that was so lacking: like yes, my [loved one] was the one who was suicidal, but I was just then sent home by myself, without any support. […] I just remember being on the phone to triage, and them saying we don’t want [loved one] to come to hospital, you just have to stay awake with [them] all night and make sure [loved one] doesn’t do anything. […] I had to get to the point of being suicidal myself to be offered any support.’
In contrast the BPD Community Family & Friends Group was described as a lifeline:
‘I felt my [loved one] fell through the cracks of the mental health system, i.e., most of the time [they were] either “too suicidal” for local support services to deal with or “not suicidal enough” for hospital admission; BPD Community helps guide you through this process.’
The unique challenges when loving someone with BPD
Relationships have ongoing and changing characteristics and are a life domain. These relationships were often not considered in the mental health system. This was experienced as a unique challenge for families and friends of someone with BPD. Upholding these relationships when relational dysregulation is a core domain of BPD, makes it extra challenging. This meant constant, daily complexity, especially for those with BPD who experienced multiple issues. This was especially isolating for families and friends when others outside the inner circle often did not understand the complexity of the relational challenges.
‘It is really isolating, because you’re coping with… it’s not just, it can be lots of things, it’s not just depression, it’s not just anxiety, not just anger, not just feeling worthless, or dangerous behaviour, it’s not just self-harming. It’s a whole lot of stuff, a whole lot of stuff so you’re not just dealing with one thing.’
One participant described this as the deeper their understanding grew, the more their insight into what drives behaviour expanded. Those who do not understand or do not want to understand, are critical and judgemental. Subsequently the judgement and stigma is likely to be felt by the family member and they feel the lack of support they themselves need. They feel blamed.
Family members especially feel guilt and grief for the life they wanted for themselves and their loved one that now seems out of reach.
‘It’s normal human behaviour to want it to not be that way. So, I would have a picture in my head of how I wanted my life to be, but in reality, it’s quite different to that. And the difference between those two set points, of what I want and what is reality, is suffering.’
The importance of changing oneself, of developing a level of awareness within oneself and in the interactions with loved ones, was emphasised: it was acknowledged that this could be achieved with the Family & Friends Group
Lifelines and Anchors
All interview participants described finding the Family & Friends Group as a lifeline in a time of need and something which they now experience as an anchor in their own journey towards wellbeing and more positive relationships. The importance of a peer group who understood was integral to their feeling safe, heard, understood and validated. It provided a foundation for impactful but challenging learning. The sense of isolation dissipated. And the sense of guilt was assuaged. The mutual sharing meant that hard truths could be heard more easily because it resonated and rang true.
‘It’s hard to put into words…I was in a place myself where I was really hopeless and powerless, and for me it changed everything. I needed some hard truths, and the people that could really deliver that in a way that I could hear it, were other people going through the same thing. […] It’s just so unique. When I was really struggling with my situation, you have your psychologist, your helplines, but there’s something just so different about it being with peers who are going through the same thing as you. You might even hear the same advice, but when it comes from someone who totally gets it, there’s something different about it and it’s so much more powerful.’
The group helped participants feel grounded and they valued the sense of community and unconditional support. The respect for the psychoeducation grounded in evidence with practical strategies, underpinned by accessible and values based theory, was emphasised.
‘If I come home and [loved one] is dysregulated, I’ve learnt not to say, ‘what’s wrong?’, I’ve learnt to say, ‘what happened?’ So that the ‘wrongness’ is not in the person, it’s something that’s going on. It might be difficult to pin down what happened, but I’m here with you, I’m not going anywhere, I can see that you’re upset, and yeah, it’s making me upset too, but what happened, maybe we can figure something out. And then they might give you a glimpse.’
Through the group, the participants were able to explore past attitudes and how they could be shifted. The subsequent shift would then have a positive flow on effect with their loved ones. Participants felt they were coping increasingly well.
Where does it lead?
In 2015 we consulted with our family members and friends of someone with BPD, this consultation led to the creation of the group. Over the years it has developed into its current form that has produced outstanding results for years. This independent research affirms that we are on the right track. Currently we are developing an online training resource and when we are funded, we hope to offer more opportunities face to face. Today the Family & Friends Group at BPD Community continues to operate each month, online. To learn about the group click here:
Family & Friends Group
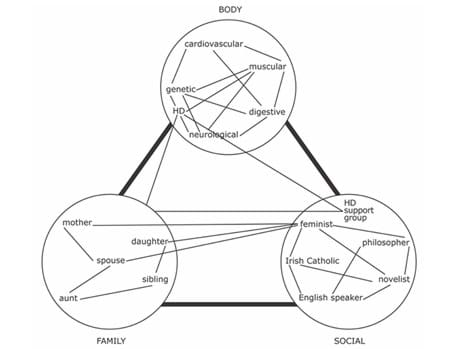
Neuroscience identifies three aspects of brain functions that affect people with Borderline Personality Disorder contributing to the development of the Project Air biopsychosocial model of BPD. We have new insight into Borderline Personality Disorder thanks to the work of Project Air, NSW.
This research informs our understanding and thanks to the work of Mahlie Jewell, a woman with lived experience of BPD, we can understand the implications of this research. In the video explaining the neuroscience, Mahlie explains what the research means to her. (click here to access the video)
Epigenetics is good news! Our brain are plastic, they can change and we can change them.
The biopsychosocial model of BPD summarises what is called the epigenetic processes of BPD. Epigenetics is the study of changes caused by the modification of gene expression. Instead of thinking about our mind as separate from our body and our environment, we can see how our mind changes, it is not fixed from birth - we are not stuck with what we are born with but are able to change how we think.
This is the best news for people who want to take control of their lives and not feel as if everything has been predetermined for them.
bio - life
psycho - mind
social - people
First we want to explain these epigenetic processes. Pre birth, our genetic inheritance is defined and we begin to feel the effects of our environment in the womb. These two factors influence each other throughout our life. However, as we all know, brain development is particularly important in the first 3 to 5 years of life, so these years lay down a framework for our brain's development.
The biological factors are infant temperament, and neurobiological sensitivity and vulnerability. This is what we inherit genetically. Then the psychosocial factors are: our attachment regulation, personality development, and our relationships and life events. These factors interact with each other and effect our 'core mechanisms'. Our core mechanisms are: 'affect' - which means our emotional regulation, 'identity' which is our sense of self, and our 'relationships' which is defined as our social cognition by the researchers - see below for more on these.
All this leads to symptoms which become pronounced usually in late adolescence and early adulthood. The symptoms are defined as: Cognitive (eg hopelessness, dissociation), emotional (eg shame, anger) and behavoural (self harm, impulsivity).
It is noted that trauma and adverse childhood experiences are a known risk factor for psychological disorders in later life. This is a complex situation because not everyone with BPD has experienced trauma and not everyone who experiences trauma develops BPD: everyone experiences a different genetic composition and a different environment. And the interactions between these unique experiences contribute to who we are. Our brain is more plastic than we once thought.
The research findings identify three areas of the brain where people with BPD seem to be different to people without BPD. Below we try to describe these simply, drawing on Mahlie's interpretation of the research.
affect
The angry amydala: tough, tiny and fierce!
This is the part of the brain that we share with our prehistoric ancestors. It is where we respond to basic emotions such as fear and we respond with: flee, fight or freeze. The neural pathways between our amydala and our pre frontal cortex (where we think logically) are limited.
When we are emotionally regulated, we control our emotional responses, we make choices as to what would be helpful for us.
The consequences of the activity in this part of the brain may also effect our sense of identity and our relationships.
identity
Negative Nancy struggles to hold on...
There are three parts of the brain that are identified in supporting our sense of identity and they interact with each other. For example, people with BPD experience a greater sense of shame and guilt and in these situations, the amydala is active for longer, increasing negative experiences.
A more negative thinking pattern develops and undermines a strong sense identity. This thinking pattern becomes a default thinking, it happens automatically even when it is obviously unhelpful.
relationships
The weird kid:
The more challenges there are in identity, the more it affects relationships. People with BPD feel criticism more keenly and they do not easily hear positive feedback. They may struggle to trust others, be sensitive to rejection and they may struggle to understand others.
So, the person with BPD stands out: maybe they don't play well with others; maybe they need to work by themselves and not in group work; maybe they need to see your face and hear your voice in order to see if you can be understood and believed. Maybe they love you one minute and hate you the next.
the good news is:
We can change our brains! It is both the easiest thing to do and the hardest thing to do.
To make the decision to change our mind is as easy as saying 'I will change my mind!' but then, the actual work is not so easy. It involves having trust in ourselves and in those who can support this change: of course, as we know, this cuts to the central dilemma of the struggle with identity and relationships.
We can think of it as a learning opportunity perhaps. If we want to learn another language, we have to practice, to study and to reflect upon the mistakes we make and celebrate the successes. They say it takes 10,000 hours before we can master a new, complex skill, like learning a language. It is the same sort of dedicated approach that we need to changing how we think, so our automatic default thinking patterns can change to become helpful thinking patterns. And realistically we need others to support us in this journey to recovery.
BPD Community creates community to support recovery.
have we been through a lot!
Problems and solutions - what can I do?
July 2022
The effects of Covid 19 have been extensive and we are not over it yet. It is no wonder we feel frustrated and anxious.
In the last 24 hours, I have heard on the radio and TV varied comments on issues that affect us deeply. Last night on TV on a panel show there was an impassioned speech about the disgraceful state of our mental health system and how you can only get attention in the public system if you are suicidal, self harming in a serious way, or assessed as a danger to others. At the other end of the scale if you have 'everyday' depression and anxiety you can easily get a mental health plan and subsidised visits to a therapist - if you can find one. For most people with a mental health issue that is not easy to treat with medication, you are abandoned by the system. It's called the 'missing middle', acknowledgement that the system does not reach the majority of people who have a mental illness. But it doesn't have to be this way.
Throw into this existing neglect a pandemic where supports have become even more limited. Social isolation means telehealth - which doesn't suit everyone. The 'worried well' are seeking psychological support for their mental wellbeing creating an increased demand on services already in stress. The health system is crushed under the weight of the demands placed upon it and the effects of a workforce falling ill to Covid and Flu and the everyday colds that are now cursing through the population as personal hygiene and mask wearing falls to the side under the guise of life as normal. It's as if everything is converging to make matters worse. But it could have been a lot worse, as a country we are doing really well.
Meanwhile there are groups within our society who have greater mental health distress: rural and regional communities, Indigenous Australians, LGBTIQ+ people, Asylum Seekers and Refugees, unemployed people. How we respond to the needs of the disadvantaged is a test of our democracy.
I am aware that in general, as a community, we are living with increasing uncertainty. We are all worried. We are worried about Covid and our kids and schools and daycare. We are worried about having a job and earning enough to get by and the effects of the war in Ukraine and petrol prices. We are worried about the superpowers flexing their muscles and challenging the status quo and climate change and energy prices. We are living in uncertainty and it cause us anxiety. The solution is found in hope and optimism, and action to make the world a better place. As always at BPD Community we look for solutions.
When we give to others without judgement that we actively practice compassion.
We can all work towards creating a kind and gentle world.
Problem 1: The Missing Middle - BPD Community has developed and is developing peer support groups with a focus on relational support and one on one coaching that can make the difference in the lives of people with lived experience of BPD. It is cost effective and one day will be the norm. We will continue to grow and develop this focus on meeting the missing middle.
Problem 2: Public health in winter - we can all take better care of ourselves with handwashing and mask wearing and not exposing others to the illnesses that we may catch. That's common sense.
Problem 3: The disadvantaged - non-judgemental compassion is essential. At a personal level we can reduce the stigma and discrimination by accepting people who are different to us and where we can, work towards creating a community where equality for everyone is important. We can be kind and we can be gentle.
Problem 4: the state of our economy and our national security and climate change - instead of being fearful of what might or might not happen, we can actively engage in our communities working to make the world a better place.
Like attracts like
May 2022
They say that like attracts like. People with lived experience of personality disorders can be attracted to each other, they are often creative and intelligent with a touch of the edginess that can make life an adventure. And they have deep loving souls and sensitivity.
Amber Heard’s diagnosis with Borderline Personality Disorder has hit the media with a bang and Johnny Depp’s legal team made much of this. It really became trial by media. The social media and internet response was enough to distress anyone affected by BPD and when people said, ‘she’s crazy, she has BPD’, or ‘I’d never date a borderline’, it was as if they were not talking about real people at all.
Creating Stigma:
The Pain in Relationships:
The most visible domains of dysregulation in a personality disorder are: emotional, behavioural and relational. People with BPD struggle with these areas of their lives and are judged if their behaviour becomes dysregulated. For women, expressions of strong emotion are looked down upon, while aggressive behaviour by men can be easily accepted. When a man behaves badly with a woman, the question often is: what did she do to provoke him?
Blaming the victim is a way of dismissing a person’s credibility and this is a common feature for people with BPD. The usual phrases are that people with BPD, in particular women with BPD are described as manipulative, liars, emotional vampires, drama queens and more. These judgemental phrases are designed to make the other person irrelevant so they can be ignored and excluded. Having BPD can be so very isolating. Blaming the victim is stigmatising.
The other most commonly known personality disorder is Narcissistic Personality Disorder. And in the same way, pejorative phrases are used to describe these people. It is interesting that we didn’t hear Heard’s legal team use that description for Depp but we did get the sense that he was controlling, dominating and manipulative. People with personality disorders can find themselves stuck between a rock and a hard place.
However, the good news is that recovery is entirely realistic and the emotional dysregulation that leads to unhelpful behaviours can be addressed with informed treatment and support and the goodwill of the person with the personality disorder. However, as long as judgemental attitudes exist, then accessing treatment and support becomes difficult.
People with BPD are highly sensitive emotionally, the hurt being done to Heard is cruel, let’s hope she doesn’t read the comments on social media. It is in close relationships that personality disorders are most tested. The very sad situation that both Heard and Depp find themselves in is not good for either of them and that which attracted them to each other in the first place is ammunition for others to use against them.
BPD Community provides support to people in relationships with people with BPD in our structured peer support group, our Families & Friends Group. The group meets monthly for support and psychoeducation, we can make a difference in the lives of family members and friends and in turn this has a flow on effect for the people in their lives with BPD. When we get funding we will do the same for people with BPD.
Watching from afar the cruelty of a traumatic relationship breakup, might be entertainment. The reality of the pain and hurt of that breakup for the people concerned is deeply sad. The flow on effect for people with a personality disorder is to reinforce the stigma and the subsequent discrimination that they feel and experience in their own lives, that is tragic especially when recovery is a realistic possibility with t.he right treatment and support: that means non-judgemental treatment and support.
Further articles of interest in this subject:
“As somebody with a personality disorder, I’m torn about Amber Heard’s public 'diagnosis'” Cosmopolitan
The Amber Heard Johnny Depp trial was an orgy of misogyny The Guardian
For every person we talk to with BPD, the question is asked:
"Where is the peer support group for us?"
I now have an answer ready, automatic:
"I am really sorry, we have everything ready to run such a group, our Recovery Club, but we can't get funding."
It hurts to be saying this with increasing frequency and it is frustrating that after such a long time, we still have not got funding to run our Recovery Club.
We currently run a Family & Friends Group, a peer led, peer support group with psychoeducation. We coach mainly family members on the skills and techniques to improve their relationship with their loved ones. This has been run since 2015, entirely by volunteers. It is managed by a Carers Committee. Last month three people with BPD tried to join the group, desperate to learn if there was anything in the group that could help them. It is heart-breaking to have to say: "Sorry, it's not appropriate for you". The content of the psychoeducation is of course totally appropriate, but it is intended for family members, so the message is phrased differently.
We owe it to our community of people with BPD to run the Recovery Club with paid professional staff. It is our responsibility to care for our people and give them the best we can, it is not appropriate for the Recovery Club not to have dedicated paid professional support. We have our Consumer Committee, we have people who can learn how to co-facilitate, deliver the training/coaching, but it is unfair to expect them, as volunteers, to undertake the responsibility of the Recovery Club and its administration. Our Consumer Committee is ready to work on the adaptation of our program and its continual improvement focus but we need to pilot the Recovery Club to do that.
So, I can hear you ask, why is it so hard to get funding? One reason is that the state government focuses its funding opportunities to larger organisations, not grassroots organisations like ours. We don't even get to apply for funding from the state government. For similar reasons we are challenged in our funding applications to philanthropic organisations. Since November last year, we have submitted eleven high quality grant applications to enable us to operate the Recovery Club, fingers crossed we are successful and can begin this work.
In the meantime, it is so frustrating for me to be constantly saying: sorry, we can't run our Recovery Club without funding to employ someone. I can only imagine how hurtful it is for our people with BPD to hear yet another rejection. If it's frustrating for me, what must it mean to them?
Lechelle and Debbie discuss their diagnosis of BPD and what it meant to them.
what's in a name?
Borderline Personality Disorder is a strange name if we think about it. Some people are relieved to get a diagnosis, others feel that the name is meant to describe them as having a personality that is wrong, while others know and feel the stigma that is associated with the diagnosis.
It is worth saying from the outset that the stigma and discrimination that we experience with BPD emanates from the mental health system and is a consequence of that system not knowing how to work with people with lived experience of BPD. At BPD Community we are pleased that this is changing, but that change is too slow for us. However, changing the name of BPD does not mean that the stigma and discrimination will go away.
In the UK, in recent years, they changed the name of BPD to include EUPD - Emotionally Unstable Personality Disorder. This is similar to the proposed name changed that Marsha Linehan suggested: Emotional Dysregulation Disorder (EDD). Meanwhile here in Victoria, there is a concerted efforted in recent times to change the name to Complex Post Traumatic Stress Disorder (cPTSD), in recognition of the role that trauma can play in the development of BPD. The American Psychological Association's definition of trauma is: "an emotional response to a terrible event like an accident, rape or natural disaster." The challenge with this change is that not everyone with BPD identifies as having experienced trauma, and treatment for trauma may not support recovery in BPD. Further, there is the International Classification of Diseases (ICD) which first defines Personality Disorders and then goes on to narrow down on BPD symptoms. The argument then becomes, whether we need to change the phrase Personality Disorders to something else. Given that co-occurring personality disorders is so common with BPD, there might be merit in that.
One challenge in changing the name is that BPD is the name defined by the Diagnostic Statistical Manual of Mental Illnesses (DSM). The document is intensely discussed and argued over by psychiatrists and clinical psychologists. When we realise that there could be as many different schools of thought in psychology as there are political parties, we can get a sense of the challenges in creating a document like the DSM.
At BPD Community we recognise the importance of getting a diagnosis because it can point people in the direction of BPD informed resources that can lead to recovery. But once the diagnosis is given, we would hope the words BPD would become meaningless unless they were used to be helpful in the ongoing discussion about how to achieve recovery for us individually. Until then, we stick to the term BPD as the official one here. We embrace the term because it identifies the people we love, those with lived experience of BPD.
living with judgement
How would it feel to read the comments made by your psychiatrists when you had been hospitalised because of your serious mental health distress. Mary O'Hagan had that opportunity.
Mary had kept a journal throughout her periods of time in hospital. She was able to compare how she was feeling in contrast with the comments made by the professionals in whose care she was kept. This contrast between the two was damning.
Mary O'Hagan is the first Executive Director of Lived Experience for Mental Health and Wellbeing, in the Victorian Department of Health. For people with lived experience this is good news. Mary's first hand experience of the stigma and discrimination experienced within the mental health sector reflects the experience of so many of us in BPD Community. This is, in part, born of the power relationship between the person with a mental illness and the treating professional. It is also part of how the system works.
We are dependent on mental health professionals who work within the medical model. The medical model views mental health and wellbeing in terms of illness, of deficit, where people of lived experience lack insight into what is wrong with them. The medical model treats the symptoms they define. People in mental distress want to be listened to and supported, they want compassion. They want recovery.
Last year Mary spoke to the Wellness Manifesto of New Zealand: "What if the Mental Health System was designed by the people who used it?" Mary's insights, born of her own lived experience and in her work as a Mental Health Commissioner for NZ, are powerful. Mary is a strong advocate for the voice of those with lived experience. To watch the video, click here
It is the total lack of connection between the hopes of those with lived experience and the practices of those who work within the medical model that highlights our perspective at BPD Community.
farewell 2021 - welcome 2022
Well, wasn't that a year!
We are living through extraordinary times where we are challenged on so many levels, and yet we have learnt so much. Individually, here in Victoria, we welcomed the end of the year as almost everyone was dragging their feet, exhausted with the trauma of the lockdown we experienced. We had barely shaken the shackles off our feet, when Omicron came along and we learnt again to live with uncertainty. As the year turns, we are walking with tippy toes, waiting to see what it means to live with COVID amongst us, unrestrained. As always we are hopeful.
Hope isn't something created out of thin air. Hope is based on experience and knowledge and understanding and change. And from little things, big things grow.
The year for BPD Community has been full of hope and change, we have built our experience and increased our knowledge. The volunteers at BPD adapted to working remotely and have tirelessly dedicated their efforts with resolve to replace stigma and discrimination with hope and optimism. Our community is ever increasing in size and we feel keenly for people with lived experience of BPD, those with BPD as well as their families and friends who seek the support of being a part of our community. Our work is done with the knowledge that we can and do make a difference.
What will 2022 bring?
We will continue to make improvements to the website. The email updates will continue to be issued monthly keeping us all in the loop. As soon as it is sufficiently safe to do so, we will return to holding our Information Nights. We have so many ideas on what to do and can't wait to see you all again.
The Family & Friends Group will continue to break attendance records while maintaining the quality of the program and its psychoeducation/training. As soon as we get funding we will be able to expand this work. The Carer's Committee works so hard in organising, administering and managing this group, they are always implementing improvements.
Our work on the Recovery Club for people with BPD continues. As soon as we get funding we will be able to implement the program, hopefully both Zoom and face to face. Our Consumer's Committee is dedicated to making this work.
All the program work and background work is done by a team of volunteers. For the first time, in 2021, we received funding to employ our Executive Officer Roy Reekie, who has hit the deck running. The Baker Foundation continues to support us into 2022.
BPD Community as an organisation is transitioning from being in start up phase to a small organisation. You can bet that we will continue to grow and continue to shake up the world of BPD in Victoria, and beyond. Happy New year to us all!
1 January 2022
challenges and opportunities
Professor Brin Grenyer of Project Air in NSW spoke recently at a research forum. He provided insight into the key concerns for people working in the field of BPD and identified three key challenges and the subsequent opportunities that these presented.
It is reassuring to know there are such dedicated psychiatrists working in the field, Prof Grenyer's team provides cutting edge research and is a powerful contribution. We discuss his three challenges and opportunities below and consider what they mean for BPD Community.
"Challenge: Research is growing – scientific studies demonstrate efficacy yet access to appropriate care is a challenge"
According to Associate Professor Rao, Clinical Director at Spectrum, about 4,000 people in Victoria receive BPD informed treatment in a year. With a prevalence of 6% in the community, that means that well over 90% of people with BPD do not receive BPD informed treatment.
"Opportunity: Developing stepped care approaches, understanding the mechanisms that impede progress"
Professor Grenyer identifies two opportunities above. These sound good, but they are in the future.
At BPD Community we are actively implementing programs to 'meet the missing middle' by focussing on the concept of 'relational support'. These peer led programs positively contribute to improving the lives of people with BPD and their families. We strengthen families so they can better support their loved ones, this has the direct effect of improving the lives of people with BPD and supporting their recovery. Our Consumer Committee is planning a pilot of the Recovery Club for people with BPD. These could fall in the category of a 'stepped care' approach. The cost of programs within the medical model are very high, by comparison, our costs are very low.
Implications for our BPD community
The challenge for our BPD Community is that the funding goes to support those who work within the medical model. Peer-led, grassroots not for profits like BPD Community, who are independent and therefore outside the medical model, are disadvantaged.
Our opportunity in this is to advocate more loudly and insistently on behalf of our community.
"Challenge: Stigma, trust and quality services are a challenge"
A resounding yes, to all three points here. In our research analysis How SaD, we learnt that stigma emanates from the mental health system itself. This is a case of physician heal thyself.
It is sad that people with BPD reach out for care and support so often and find the doors closed to them. In the study undertaken by Associate Professor Rao, most people with BPD who suicide reach our for help prior to their suicide. That appropriate care is not accessible is a result of stigma and discrimination.
Implications for our BPD Community
The challenge for our BPD Community is that our voice is the voice of lived experience and is easily overlooked. Our mission is to replace stigma and discrimination with hope and optimism.
Our opportunity is to develop our organisation until we can no longer be overlooked but can work with our colleagues in the medical field to achieve our mutual objectives: to support people with BPD and their families and friends.
"Opportunity: listening to lived experience, improving care, and developing peer work roles"
The recent Royal Commission into the Mental Health System in Victoria prioritised the voice of lived experience both for people with BPD and their families. But here's the rub. This is what working within the medical model means: lived experience is listened to, it doesn't drive the change. Developing peer work roles within the medical model is to create a workforce to fit the bottom of the hierarchy of importance in the highly structured workplaces of hospitals and other medical organisations.
"Challenge 3: We mostly only know about borderline disorders"
BPD is one of the least researched mental illnesses, yet the research into BPD is greater than the research into other personality disorders. Yet other personality disorders present for people with BPD. The recent International Classification of Diseases has produced the best explanation of what Personality Disorders are and what BPD is. The DSM is so outdated and is more than clumsy. Narcissism is a very common feature of our society today, where does the relationship with this and Narcisistic Personality Disorder begin and end.
"Opportunity: Deepen knowledge and work into other problems such as pathological narcissism"
Hmmm. Yes it would deepen knowledge, yes it would be helpful to learn and understand. This however presents more challenges. BPD is currently still so misunderstood within a large proportion of the medical and psychological field. Will this add to the confusions? I expect that the advantages far outweigh the cons. Enough people with BPD also struggle with narcissism to varying degrees, more knowledge would be helpful for their recovery.
Implications for our BPD Community
The challenge for us is in the question, does this distract from our concerns for people with people with lived experience of BPD? As an organisation it is not feasible for us to change, however, this might be an issue to address in the future.
The opportunity is that the more we can learn about what personality disorders are and the different features of them, we can better understand BPD also. This means we could continue to develop and improve our responses to provide support and care for our BPD community.
We would like to take this opportunity to thank Professor Grenyer and his team for the excellent research that contributes to positive changes in the world of BPD. Much has been achieved since we arrived on the scene in 2015, and there is much more to go, meanwhile we are reassured that the dedication of people like those at Project Air will contribute to even more change for the better.
national children's mental health strategy
Often when a child reaches adolescence, the multiple factors of puberty, familial and social expectations mix with vulnerability in mental health. When they collide, the foundations of a future with mental illness is created.
There are so many reasons to focus attention on to the mental health and wellbeing of our children and with the release of the National Children's Mental Health Strategy, we hope there will be change ahead; after all, our children are our future.
In families around Australia children experience poor mental health: sometimes they are coping with parents who are struggling with mental health problems, sometimes the children themselves are challenged with mental health concerns.
Focus area 1: Family and Community Priority actions:
Increase parent and carer mental health literacy and their skills to support child mental health and wellbeing, via:
• Routine offering of evidence-based parenting programs at key developmental milestones (action 1.1.c)
• Emotional wellbeing modules embedded in antenatal and parenting courses (action 1.1.f)
• Widely accessible evidence-based resources building on existing initiatives (action 1.1.b)
• A national campaign promoting the value of parenting programs (action 1.1.d).
Support communities with the highest levels of need to address social and economic disadvantage (action 1.3.a) through:
• Implementation of tailored programs focused on improving children’s mental health and wellbeing based on the key characteristics of successful place-based approaches (action 1.3.b).
Focus area 2: The Service System Priority actions:
Improve the capacity of systems to deal with complexity through:
• Trialling (networked) sites in both urban and rural areas of a service model of integrated child and family care that exclusively provides holistic assessment and treatment for children 0-12 years old and their families (action 2.1.c)
• Trialling sites with innovative service delivery models that integrate face-to-face and telehealth consultations, digital interventions, and phone helplines (action 2.3.c)
• Providing support based on genuine co-design with children and families involved in the design, delivery and evaluation of services (action 2.3.e)
• Allocating funding for care coordination for families with complex needs (action 2.4.a)
• Requiring all government departments to outline and regularly report on what they do to support children in State care (action 2.4.d), providing priority access to relevant services (action 2.4.c).
• Amend current Medicare items to promote collaborative care including:
• Enabling all providers (regardless of discipline) to claim for case conferencing (action 2.2.a)
• Enabling providers to claim for consultations with parents and carers (without the child present) as part of the child’s care (action 2.2.c)
• Requiring providers to communicate with educators and other service providers about a child’s treatment and support plan (action 2.2.d)
Focus area 3: Education Settings Priority actions:
Ensure educators are well-equipped to support child mental health and wellbeing by:
• Requiring all early childhood learning services and primary schools to have a comprehensive wellbeing plan for their students (action 3.2.a)
• Providing funding to implement quality improvement activities and delivery of evidence-based programs targeting needs identified in wellbeing plans (action 3.2.b, 3.2.c)
• Having a designated wellbeing staff member in all early childhood learning services and primary schools who is responsible for planning and coordinating wellbeing activities, including the development of wellbeing plans (action 3.1.b, 3.1.c).
Focus area 4: Evidence and Evaluation Priority actions:
Ensure better collection and use of data through:
• Establishing Inter-Departmental Committees to resolve current barriers to relevant data sharing across sectors such as education, justice and community health, for the purposes of informing child mental health and wellbeing (action 4.1.d)
• Embedding evaluation in program and service delivery from the beginning, with reporting of findings required to receive further funding (action 4.2.a)
• Including implementation evaluation as a core component of programs delivered in schools and early childhood learning settings to identify what is required to ensure fidelity (action 4.2.c).
• Require supports to be based on and continue to involve high-quality research and evaluation through:
• Funding parity for child mental health research and child physical health (action 4.3.a)
• Targeted funding allocated on the basis of priorities including gaps in current treatment knowledge and the needs of priority populations (action 4.3.b).
In conclusion, at BPD Community, we know only too well that the proof of the pudding is in the eating. When and how these actions are implemented is when and how we can tell if there will be a better future for our children. This strategy is a promising start for a different approach.
celebrating hope and optimism - Oct 2021
At this time every year we celebrate.
We celebrate recovery - the journey of people with lived experience of BPD and their recovery is worth singing out loud about;
We celebrate the work and our achievements over the year this is our second year working within the limits of Covid restraints and we are thriving. We have a grant from the Baker Foundation to provide the basis of our sustainability;
We celebrate those who volunteer and those who work with BPD Community to make this possible. It is from the work of so many people contributing so much that gives this organisation its strength.
Discover creative wellbeing
This is the theme for BPD Awareness Week this year. This theme recognises that the support for people with BPD extends well beyond the concept of therapeutic treatment. At BPD Community, we are dedicated to meeting the missing middle with our focus on relational support and the provision of peer group support and psychoeducation and training. Our work is informed by the evidence of lived experience.
stigma and relational support
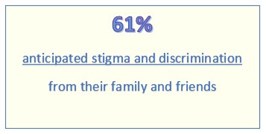
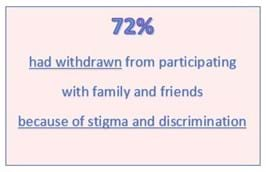
Dr Chris Groot's most recent research has been into stigma. With SANE Australia, Dr Groot investigated stigma and mental illness from the perspective of people with a mental illness. 'Our turn to speak' was a survey undertaken between October 2019 and March 2020 of about 2,000 people with a mental illness. The results of this survey were published in the National Stigma Report Card
It is timely to revisit this work which was published during last year's BPD Awareness Week.
The research into stigma and discrimination from the experience of people with a mental illness produced some shocking results. Families and friends of someone with BPD might feel defensive with these results, they do indicate that a judgemental approach from a family member can add to the severe distress that a person with a BPD is feeling. However there is good news in that positive relationships are recognised, and sad news that so many have found it necessary for their mental health to withdraw from close relationships that should be supportive.
People with BPD "...are all too frequently excluded by mental health services..."
Read Dr Groot's article on Stigma and Discrimination from last year's BPD Awareness Week. Sadly it is still relevant today BPD: It's time to change the narrative
The Baker Foundation has invested in our future so we can to implement the Sustainability Project. Thank you Baker Foundation.
The work for this year is to do what we can to ensure sustainability for the future so we can implement the many programs and projects we would like to. We have employed a part time BPD Community Manager, Daryl Taylor and a Fundraising Manager, Steve Jacobi and we welcome Daryl and Steve to our community.
BPD Community is proud to operate outside the medical model and the restraints of being a part of a medical approach to BPD. Our focus is to create a community to support recovery through relational support. We do this through peer support and psychoeducation.
As the only independent BPD organisation in Victoria, we rely on the support of those who believe in our mission to replace stigma and discrimination with hope and optimism and our vision of a compassionate community. Thank you to those who have donated and who continue to support us.
Our priority programs are peer support groups for both people with BPD and their families and friends as well as training programs that will support their learning. We have ambitions and great expectations for what we could do with funding, as we move from being run by volunteers, to having paid staff. Thank you to the volunteers who have, over the years, provided support and encouragement to the people of our BPD Community. We look forward to continue working with our volunteers as we move forward into the future.
Relational regulation
It is the experience of BPD Community that a focus on 'relational support' enables people with lived experience focus on recovery. The work we do is psychoeducation, individually tailored, with a view to build relationship skills. In this way we address emotional, behavioural and cognitive dysregulation. How this supported the key domain for people with BPD that is identity dysregulation, was hard for us to explain, until we learnt about the groundbreaking work done in this area that explores what it means to be a 'networked self'.
identity regulation
People can have a fractured sense of self when they feel defined by others in a particular way. So, if a person experiences the stigma and discrimination of BPD, they might feel objectified or reduced. It is "It is the inappropriate, arbitrary or unfair salience of a trait in a context". There is much to learned from this different approach to identity.
for more information read the article here: You are a network
55 recommendations - what do they mean?
It's not a revolution, it's a reform with a long view.
There will be some immediate changes in the public health system but for people at the ground level, people with lived experience of BPD (consumers and carers), the immediate changes will not be so obvious. One big immediate change has been the creation of Mental Health Reform Victoria who is responsible for implementing the recommendations of the Royal Commission. And what those 55 recommendations do is begin to lay the groundwork for long term change.
It was in the 1980s that the mental health asylums in Victoria were closed down. The focus was supposed to be on support within the communities where people lived. Today we have a mental health system where there is little support in the community and instead the focus is on a waiting list for treatment for those who can access hospitals when their illness is serious and complex. If you have the money you might be able to get private treatment. Those with BPD who have lots of money might even go to USA for treatment. The recommendations are designed in part, to provide that community support that is so lacking. For people with BPD, this is good news...in the long run.
A key focus for the reform is the participation of people with lived experience in the process. There is an emphasis on peer worker development and peer participation, to encourage people with lived experience (people with BPD and their families and friends) to be more actively involved in determining how the system works. The long term goal will be a mental health and wellbeing system run by people with lived experience. Again, this is great for the long term reform that is needed.
The challenge for people with lived experience of BPD, is the stigma and discrimination that exists. This means things like we don't even get counted as a mental illness in the National Mental Health Commission data, but we do note that in their report of 2019, they did commit to a feasibility study to investigate options for expanding the scope of disorders and high risk community groups. So, things are changing here too.
In the short term, there is enough work to keep BPD Community busy filling the gaps that currently exist in the system and advocating for the necessary changes to replace stigma and discrimination with hope and optimism. For us, it's life as usual.
the report card says fail. time for reform!
The Victorian Mental Health System operates in crisis mode: only those who are at high risk get access to treatment.
The reforms announced yesterday by the Royal Commission are about placing the community at the centre of mental health and wellbeing. BPD Community welcomes the report and looks forward to continuing to be be a part of the solution.
The Final Report of the Royal Commission into Victoria's Mental Health System identify 65 recommendations and five volumes outlining the reforms, see below:
The system’s failures can be linked to its origins. In the 19th and 20th centuries, people living with mental illness were separated from the rest of the community and housed in institutions. These institutions began to be dismantled from the 1980s, with a desire to move towards a community-based model of care.
While there has been social change since then, such as a strengthened focus on protecting and promoting human rights and the consumer movement, Victoria’s mental health system has not kept pace. It has drifted away from its earlier aspirations of a community-based system and now relies too heavily on hospital‑based services and emergency departments.
BPD Community has struggled to work in this broken system and has successfully shown what can be done with an innovative, flexible and efficient approach to community based responses that include all people with lived experience.
We remain hopeful and optimistic that our work can now be extended so we can support more and more of our BPD community in their individual journeys to recovery. We will continue to focus on relational support, building our sense community and peer led support at a grassroots level.
BPD Community is proud of the work it does we have been a part of the reform and will continue to lead the way on behalf of our community of people with lived experience of BPD.
hold onto your hat!
The Victorian Royal Commission into Mental Health
in November 2019 produced an interim report,
in February 2021 will publish it's final report.
What can we expect?
THE THEMES THAT EMERGED:
- Investment in the system is poor.
- Getting help is difficult.
- Access to services is not egalitarian.
- The ‘missing middle’ miss out.
- Emergency departments as entry points of care.
- Dignity is often disregarded.
- Stigma and discrimination are ever-present.
- Our younger people are adversely affected.
- Families and carers are left out.
- Mental illness is even more complex for some groups.
- The mental health of Aboriginal communities.
- Suicide.
- Recovery.
- Trauma is unseen.
- The system is driven by crisis.
- Demand has overtaken capacity.
- Prevention.
- It is different outside Melbourne and in the bush.
- Alcohol and other drugs add another dimension.
- The workforce.
INTERIM RECOMMENDATIONS:
Recommendation 1: Establish a Victorian Collaborative Centre for Mental Health and Wellbeing
Recommendation 2: Targeted acute mental health service expansion
Recommendation 3: Suicide Prevention
Recommendation 4: Aboriginal social and emotional wellbeing
Recommendation 5: A service designed and delivered by people with lived experience
Recommendation 6: Lived experience workforce
Recommendation 7: Workforce readiness
Recommendation 8: New approach for mental health investment
Recommendation 9: The Mental Health Implementation Office
and then COVID entered the scene!
the publication of the final report was postponed to Feb 2021
The Royal Commission went online, BPD Community submitted another response following the release of our Position Paper on Prevalence, we spoke in a focus group and individually.
We await the final report of the Commission in anticipation that people with BPD get what they need and in recognition that it won't happen overnight. We also wonder what the Commission report will mean for organisations such as our own BPD Community.
create A Person‑Centred mental health system
We want change, the Productivity Report just released to the public doesn't challenge the existing system, its the existing system that fails us.
The report recommends that 'governments should create a mental health system that places people at its centre'. Yet it confirms the medical model at its centre.
It says: "The needs, preferences and aspirations of the people who use the system, as well as their families and carers, should shape all parts of a person-centred system — from the work of the individual clinician to the policies proposed by decision makers — to create recovery-oriented services and supports."
and, "A person-centred mental health system would enable people to access the combination of healthcare and community services that will best help them to recover from mental illness and to achieve the outcomes that matter to them. People should be empowered to choose the services most suitable for them, and these services should be evidence‑based and responsive to their cultural, social and clinical preferences".
The Productivity Commission recommends a nicer version of the same thing.
demand a compassionate mental health system
The mental health system is broken said Dan Andrews when he announced the Victorian Royal Commission into Mental Health in 2018. The Commission will report back early next year. But, "the crisis in mental health is now", says Professor Ian Hickie, in response to the effects of COVID 19.
So let's look at some facts:
1) Suicide rates are about the same as they were last year. There has been no increase in suicide but suicide rates have constantly increased since 1980. Access the data here.
2) Calls to crisis phone lines increased by 67% this year.
3) Action on the BPD Community Forums managed by SANE from March to June this year, increased by 118%.
In response to this overwhelming need, the federal government increased subsidised psychology sessions by 10 sessions to 20 a year. And both state and federal governments pumped money into existing mental health services. They are doing more of the same and expecting different results and creating pressure on the system. Waiting lists are increasing and BPD informed care is still generally unavailable.
What we are experiencing is the effect of our COVID 19 times on those with pre-existing mental health issues. Given about 1.1% of people with BPD get treatment for BPD in a year, does this surprise us? Hundreds of thousands of people in Victoria with BPD are ignored by the system. We need to use our voice where we can to demand a compassionate mental health system.
position paper on prevalence - October 2020
BPD Community accepts a prevalence of Borderline Personality Disorder (BPD) in Victoria of 6%. This is based on an analysis of the research discussed in the Position Paper on Prevalence presented here. This figure includes people who would be sub threshhold, or 'diagnostic orphans' those who live with what might be considered a moderate level of disorder.
This means about 350,000 Victorians who have BPD and about 700,000 family members. One in six Victorians are affected by BPD. This is shocking. When we consider that about 4,000 people a year receive treatment for BPD, it is disgraceful.
BPD Community has a mission to replace stigma and discrimination with hope and optimism and we are working hard to make change possible.
Social isolation limits the support we receive informally from others.
A study just published by VMIAC a Victorian consumer organisation showed what we would expect: under 35 yr olds have been most severely affected by the constraints of COVID19, social isolation in particular.
What these results show is that for people with a mental illness, their relationships are so important to them, they give vulnerable people a sense of support and belonging. This reinforces BPD Community's focus on developing skills and relationship building for people with BPD and giving families and friends the skills needed to improve their relationships with their loved ones.
To read more about the report click here.
the effects of covid-19 conditions on people with eating disorders
Swinburne University has completed a study on the effects of COVID-19 conditions on people with eating disorders. As we could expect, people with eating disorders, like the rest of us, have found it a challenging time. One could predict that people with eating disorders would find it more difficult to manage their mental health under the added anxiety of the uncertainty of our times. Many people with BPD experience eating disorders, so this affects our BPD Community too.
“These results show that even during the very early stages of this pandemic, (roughly three weeks after the official announcement by the World Health Organisation), this group of people were already reporting spikes in these behaviours. This could have been due to increased stress, anxiety and depressive symptoms as a result of social distancing measures,” explains Dr Andrea Phillipou, a co-author of the paper commented.
The need for increased mental health support has been reinforced again.
more than meets the eye
The BPD mask is how we hide from the really world how we really feel. Sarah describes the feeling of social isolation that people with BPD experience everyday. On the surface everything appears normal, below the surface is a cruel, debilitating psychic pain.
BPD Community is a place where people can feel accepted, where they belong. But there is so much more that can be done. We at BPD Community are striving to do the simple things that can make such a big difference. You can help us, you can join our community.
This powerful, challenging video shows us that there is more than meets the eye.
Supplementary Submission to the victorian royal commission
Just our luck! The COVID-19 restrictions hit the week we were to speak with the Victorian Royal Commission into Mental Health. At that meeting we were preparing to explain our Theory of Recovery and the solutions we proposed to the current sad state of affairs that exists in relation to BPD.
We have since heard that those meetings have not been postponed as originally planned, but are now cancelled. So, we have revisited the work we have done on this to to try encapsulate the essential elements and prepared the Supplementary Submission which you can access by clicking on the image opposite. We hope you appreciate it and if you have any questions or comments please contact barb@bpdcommunity.com.au
What works?
It was a totally engaged audience at the last Info Night where Elise Carotte presented to the community the knowledge of what treatments are most commonly available in Victoria and why they work. She also provided a slide of where treatments can be sought in Victoria (note this last information is subject to change). Her slides are available for you - click on the picture opposite to access them.
mental health across the lifespan conference
On Tuesday 17th and Wednesday 18th of March, there will be a gathering of people to discuss the question of mental health across the lifespan in Victoria. There will be many important figures in the world of mental health of today. Minister Foley will be there, Pam Anders, the CEO of the new Mental Health Reform office in Victoria will be there, Dr Stephen King, the chairperson of the Productivity Commission into Mental Health will be there and heaps more people who are the decision makers in the field that directly affects us.
Also there will be people with lived experience both people with BPD and the families and friends. Mental Health Victoria has generously given BPD Community free tickets to allow our people attend. If you are interested in attending, please contact Barb at barb@bpdcommunity.com.au or on 0409 952 754, so she can explain what to do.
BPD Community speaks to Productivity Commission
What a difference it would make if people with lived experience of BPD who have access to BPD informed treatment, social supports (eg employment supports) and relational supports (eg peer led support groups and psychoeducation).
On 18 November BPD Community spoke to the Productivity Commission to critique its reliance on the medical model and complete rejection of the concept of relational supports and have prepared a supplementary Submission to the Productivity Commission (see link opposite) based on that presentation.
Consider who is there for the person with BPD 24/7: it is the family and friends who are there whether or not a person is in treatment and currently less than 2% of people with BPD are in treatment. Most people with BPD are unsupported and this is a shocking neglect. With training in psychoeducation, family and friends can learn how to better support their loved ones and people with BPD can continue to work on their own recovery. The Productivity Commission makes no acknowledgement of this and it is a glaring omission. Relational support for people with BPD and their families and friends is essential.
bringing families into the picture
Families are an essential element in the recovery process, they are there 24/7 for their loved ones. Including families in the recovery process is crucial to improve outcomes for people with BPD.
Professor Daniel Flynn, Ireland Dr Mary Kells, Ireland and Professor Robert Krueger, USA, are speaking at the one day Conference on 'Bringing Families into the Picture'. Costs are: Clinicians $295; Family members/Carers $145; Young People/ Concession $60. Click on image opposite for conference flyer.
NEA.BPD (Aust) is the Australian branch of the National Education Alliance of USA. They run the Family Connections program here and have sponsored some excellent training of professionals, such as bringing out Dr Alan Fruzzetti who is an expert on Dialectical Behaviour Therapy.
Orygen provides specialist mental health services for young people aged 15 to 25 who reside in the western and north-western regions of metropolitan Melbourne. Orygen is dedicated to helping young people early.
Victorian royal commission into mental health - interim report
The Royal Commission acknowledges that mental health is shaped by the social, cultural, economic and physical environments in which people live and is a shared responsibility of society.
It envisages a mental health system in which:
1. The inherent dignity of people living with mental illness is respected, and necessary holistic support is provided to ensure their full and effective participation in society.
2. Family members and carers of people living with mental illness have their contributions recognised and supported.
3. Comprehensive mental health treatment, care and support services are provided on an equitable basis to those who need them and as close as possible to people’s own communities—including in rural areas.
4. Collaboration and communication occur between services within and beyond the mental health system and at all levels of government.
5. Responsive, high-quality, mental health services attract a skilled and diverse workforce.
6. People living with mental illness, their family members and carers, as well as local communities, are central to the planning and delivery of mental health treatment, care and support services.
7. Mental health services use continuing research, evaluation and innovation to respond to community needs now and into the future.
Productivity Commission - Interim Report
The Productivity Commission interim report was released at the end of October. It says that we spend $18 billion on mental health but that it accounts for $51 billion in productivity costs. The Interim report identifies 5 key areas of reform:
Reform area 1: prevention and early intervention for mental illness and suicide attempts.
Reform area 2: close critical gaps in healthcare services eg the right treatment for their condition.
Reform area 3: investment in services beyond health, eg housing.
Reform area 4: assistance for people with mental illness to get into work and enable early treatment of work-related mental illness.
Reform area 5: fundamental reform to care coordination, governance and funding arrangements
The Interim Report and related documents can be found here: https://www.pc.gov.au/inquiries/current/mental-health/draft it will be possible to make submissions to this report by Jan 2020.
BPD Conference in Melbourne
The theme is the conference this is is: Best Practice Deserved. The key note speaker is Professor Jayashri Kulkarni who was recently featured in an article in The Conversation, proposing that BPD be reconsidered as Post Traumatic Stress Disorder.
The first day of the conference, Thurs 14th Nov, is dedicated for professional training at Spectrum, the second day, Fri 15th Nov, is for people with lived experience, both consumers and carers, as well as those who work with BPD. Day 1 costs $145 for those in the not for profit sector, $195 for other professionals; Day 2 costs range from $20 for those with lived experience on a concession card to $250 for professionals working in the sector. The post conference networking event costs $30. Day 2 is at the Bayview Eden, Melbourne.
Coping with self harm
'I don't know what to do, I feel helpless' is a common cry for families and friends whose loved one self harms. There is a short simple booklet written in easy to understand language now available for free from Orygen.
There are lots of simple techniques that can be immediately applied, it is a booklet with answers. It is reassuring to know that, "Although some people who self-harm may be suicidal, self-harm is often used as a way of managing difficult emotions without being a suicide attempt".
To download the booklet, click on the picture at the right and complete the form to be transferred to the page to download.
Royal commission into mental health - teresa's statement
Teresa is a woman who has lived with BPD for all her adult life util she recently found the support that would help her navigate both the system and her own personal challenges. It was following a period of hospitalisation that she was assigned a 'friend' who could provide non judgemental support and this friend held Teresa's hand for the next six months.
Teresa was shocked at the challenges she had faced, while she struggled to understand what was happening. She had done well at school and university, graduating with a medical degree. All was in place for a good life, except she had BPD. Click here to read Teresa's statement.
Royal commission into mental health - nicole's statement
Nicole describes herself as high functioning, she is successfully attending University, completing a degree in nutrition. She is just 22 and very brave. She spoke to the Royal Commission about her experiences in the mental health system. She was still at school when she was going to Headspace, she has now moved into the adult system and sees a psychologist for those 10 visits a year which is patently not enough and supplements this with a visit to the Uni Counsellor, she calculates she has 1 hour a month. This is of course not enough for a structured treatment program.
Tellingly, Nicole speaks about the distress of finding out that she was given a diagnosis of BPD, when or by whom she does not know. Her story can be read on the link opposite, we highly recommend it.
Royal commission into mental health - the system
This is a brief explanation of the Mental Health system in Victoria. The short video opposite describes 4 levels:
1. Primary health Care, eg the GP
2. Community Support and Clinical Services eg BPD Community, your Community Health Centre
3. Specialist Clinical Services eg Spectrum
4. Crisis Care eg Emergency Dept of your hospital, Lifeline, 000
There is acknowledgement in this official video, that the system is broken. The issue now is, how to fix it. That's what the Royal Commission is about.
royal commission into mental health - hearings
Read Teresa's testimony to the Royal Commission. Her eloquent explanation of what BPD felt like for her is deeply moving.
She said it was after the last hospitalisation when she was assigned a 'friend' to support her and ease her way back towards recovery, that she was finally able to get on track. Click opposite to access the transcript.
The Royal Commission is conducting public hearings at the moment. You can watch them live, I highly recommend it to anyone with an interest in mental health. click here to access the live stream.
Royal Commission into mental health - submissions
The Royal Commission is accepting submissions now. However, if you are not accustomed to writing, it can be a daunting experience. There are some simple rules to help you make the best submission you can. This might take a few hours of work over a few days, so be prepared to give it the time it needs. The Commission is listening to us so we want to give them the best information we can. BPD Community wants to encourage ALL our people to make a submission (click on picture to the left). I have used examples that we know to show you how to do it.
A. Read and think as much as possible about what the commission says (click above). To make a brief submission (about 500 words or less) you have a choice of responding to 6 'questions':
- How can the Victorian community reduce the stigma and discrimination associated with mental illness?
- What is already working well and what ideas do you have to better prevent mental illness and to support people to get earlier treatment and support?
- What ideas do you have to prevent suicide?
- What makes it hard for people to experience good mental health and what can be done to improve this? This may include how people find, access and experience mental health treatment and support and how services link with each other.
- What areas and ideas for change would you like the Royal Commission to prioritise?
- Is there anything else you would like to share with the Royal Commission?
B. Draft a rough copy
- Think about one message you want the Commission to hear from you. Try to sum it up in one or two sentences.
eg "I think the Emergency Dept needs to improve how it responds to people who are suicidal." or
eg "I think the police don't always respond appropriately." - Think about examples, incidents or experiences that can explain why you think as you do. Note the time, the place and the people involved are helpful to say at the start (when, who, where)
eg "In 2017, I went to (you can name the hospital) emergency because I was suicidal."
eg "In 2018, my daughter was high on ice, the police cornered her in the toilet of our home and then capsicum sprayed her." - Then explain why this was a problem.
eg "I was discharged 3 days later, with three temazapan. No follow up plan, no referral. I don't really remember much, I was really distressed at the time. I was 17. I didn't know what to do. I didn't have anyone who would look after me."
eg "I was really worried for my daughter. She was really difficult for us. Another time when the police came, they were really good but this time they were pushy. My daughter was petrified, screaming with fear and then they capsicum sprayed her."
C. Reflect on what you have prepared, is that the best way to communicate what you want? Could you say it better? Could you use a different example? Which question does it fit best?
- The first example is easily fits the question on suicide (qtn 3) you would then want to consider what could have been done better, eg a referral to a mental heath service; a diagnosis; follow up after discharge. It could be used in qtn 4 also.
- The second example could be an example of stigma and discrimination if you thought the police were unfair. It could also be used in response to qtn 4.
Go from B to C as many times as you like with as many situations as you want taking care not to repeat yourself. You might want to make a list of different messages using one or more examples or you might want to make a list of examples to illustrate one message. The thing to ask yourself is "Am I communicating what I want to say?"
You might want to discuss your response with someone you trust and ask them to help you. You can ring Barb at BPD Community on 0409 952 754.
D. Now you are ready to begin your response:
- write a your response out.
- read it carefully or get someone else to read it
- fix your mistakes (we all make typing mistakes, grammar mistakes) we want this to be the best possible piece of writing we can do.
E. Copy and submit your response (access the site from the link above). Make sure you have a copy of what you write so you can read it later. Celebrate your achievement! It is not easy.
Royal Commission into mental health website
The Royal Commission into Mental Health has hit the ground running! They had set up their website (see on right) and determined a whole lot of times to travel around speaking to people. They are visiting rural, regional Victoria and suburbs in Melbourne too. This is the best time to go and get a sense of what is happening and they will be listening to what people say.
If you want things to improve for our BPD Community, this is a chance to speak your own experience and have a say.
All about bpd
SANE has published an excellent paper on BPD exploring all the challenges and contradictions and confusions that exist here in Australia in relation to this diagnosis and that of other personality disorders. It indicates the need that exists for an Australia hungry for information on BPD "in the 12 months to 31 July 2017, 22% (230,000) of all users (1,048,000) who visited SANE’s online platforms accessed materials on BPD, including factsheets and other information".
The paper is a weighty discussion of the situation in Australia regarding all Personality Disorders, with a focus on BPD. It is a solid read requiring a pencil in hand, a comfy chair and a fair bit of time. The rewards are considerable if you make the effort.
Royal commission into mental health
The composition of the Royal Commission into Mental Health was announced this week. The Chair will be Ms Penny Armytage, fellow Commissioners are: Bernadette McSherry, Professor Alan Fels and Associate Professor Alex Cochrane.
They will produce a preliminary report this coming November and a final report by October 2020. The government has committed to implement every recommendation but it is understood that this will all take time.
The Terms of Reference have been finalised. We will make them available shortly.
For further information the ABC report is informative: click here
Our Opportunity for Change - Info Night
The mental health system is a bit of a mess. Would you like to have input into the changes that are so necessary? The Royal Commission into Mental Health is our chance to get things changed. This is the best good news story we have had for a while, we have the chance to do something that will have direct impact on the lives of all of us affected by BPD. The best way to change things is to work with others. Come and join how we can begin to learn how to do this this coming Wednesday, 27 February at 6.30. The speaker is Angus McLelland, CEO of Mental Health Victoria and the venue is at the offices of Mental Health Victoria, level 2, 22 Horne St, Elsternwick: rsvp to barb@bpdcommunity.com.au
Click on the flyer for more info
Media Release Preventing Suicide In Local Communities
The Andrews Labor Government is set to roll out stage two of its Suicide Prevention Framework to support local communities to reduce the stigma by giving Victorians and their families the support they need.
“How SAD” Stigma and Discrimination of People with Borderline Personality Disorder (BPD)
Stigma is a mark of disgrace associated with a particular circumstance, quality or person. Stigma sets people apart. Discrimination is the unjust or prejudicial treatment of different categories of people. Discrimination is the effect of stigma.
How to be happy
The art of making yourself happy is something we can all learn and practice. No one is happy 100% of the time. Life has its ups and downs. Even so there are some sure fire ways to increase your happiness. Published with the permission of Andrew Fuller www.andrewfuller.com
BPD Community Newsletter Vol.1, Issue 10, February 2017
BPD Community Newsletter Vol.1, Issue 10, February 2017
Diversity is the art of thinking independently together. No, this is not an oxymoron but a deeply philosophical commitment that underlies BPD Community. We are such a diverse community on many levels and we are united in a common purpose with a common vision
BPD Community Newsletter Vol.1, Issue 9, October 2016
Each day we become increasingly aware of how much more can be done to replace stigma and discrimination with hope and optimism. At this time of year it is appropriate to look back and reflect on our work
BPD Community Newsletter Vol.1, Issue 8, August 2016
It seems every time we turn around there is a reason to celebrate.
This issue reports on our recent Info Night, a Family Affair, dedicated to Carer initiatives. Inside you can read about the latest Guiding Principles for carers.
BPD Community Newsletter Vol.1, Issue 7, May 2016
To replace stigma and discrimination with hope and optimism is a challenge. Stigma and discrimination affects all of us and it requires all of us to work together to bring hope and optimism. So how we create this change we want, requires us to consider exactly what is it we want to change
BPD Community Newsletter Vol.1, Issue 6, March 2016
Summer seems to come on in a rush and by the time you recover from Christmas and holidays, everything just happens in a rush. We have hit the ground running this year.
BPD Community Newsletter Vol.1, Issue 5, October 2015
When you’re having fun, time passes quickly and our first year has been and gone.
Creating a sense of community is central to our work: clinicians, carers and consumers, we are united in our desire to replace stigma and discrimination with hope and optimism
BPD Community Newsletter Vol.1, Issue 4, Sept 2015
Living in the present means living with change and our BPD community is no exception.
Our biggest news is the launching of our BPD Community Facebook page. Just google BPD Community and it should appear.
BPD Community Newsletter Vol.1, Issue 3, June 2015
We all know that giving birth can be both a painful and rewarding experience. And after the birth, we all think the newborn is the prettiest, most handsome of all children ever born. Well some of us do at least, - and so, we think our BPD Community baby organization is the best baby ever!
BPD Community Newsletter Vol.1, Issue 2, February 2015
a lot in such a short time. Starting a new organization is challenging. There are, it seems, four phases to any organization: forming and storming., norming, performing . Well, we’re doing all four at once it seems.
BPD Community Newsletter Vol.1, Issue 1, November 2014
We are indeed over the moon! On Wednesday the 5th November an executive to the Victorian branch of the Australian BPD Foundation was elected. And what a group of people we have to represent the interests of our BPD Community.